Health authorities from all around the globe are hurrying to examine the stockpiles of vaccinations and treatments that may be required to prevent the spread of monkeypox, which has already broken out in more than a dozen different countries.
According to statements made to the media by authorities from the Centers for Disease Control and Prevention on Monday, the United States’s emergency stockpile now has two vaccines that have been given the all-clear by the Food and Drug Administration as being effective against monkeypox.
The stockpile includes more than one hundred million doses of the smallpox vaccine that was used initially. However, this vaccination is linked to a number of adverse effects and should not be administered to some people, especially those whose immune systems are already impaired.
In 2019, the FDA authorised the use of a more recent vaccine called Jynneos for the protection of both smallpox and monkeypox. According to Dr. Jennifer McQuiston, a deputy director at the Centers for Disease Control and Prevention, the stockpile has more over one thousand doses.
Despite this, the scope of the issue in the United States is not yet completely understood. As of Monday, the authorities had only verified one case, which was found in Massachusetts, and were conducting evaluations on four other cases.
The situation in other countries is of more concern. As of this past Monday, there were over one hundred confirmed cases in fourteen nations outside of Africa, with dozens more cases now being investigated. On that day, the European Center for Disease Prevention and Control asked health professionals across Europe to evaluate the availability of smallpox vaccinations, antiviral medications, and personal protective equipment.
There are around 31 million doses of smallpox vaccine in stock at the World Health Organization (WHO), although it is possible that they have lost part of their efficacy in the decades since they were manufactured.
The biggest clusters of monkeypox cases have been documented in Europe, namely in Spain. As a result, a number of knowledgeable individuals have come to the conclusion that the epidemics started in Spain. Both a sauna in Madrid and a Gay Pride event that was hosted in the Canary Islands starting on May 5 and attracting over 80,000 revellers are under investigation by the Spanish authorities as possible causes of the outbreak.
A little more than a week after the first outbreak in the Canary Islands, the United Kingdom reported its first cases of monkeypox in individuals who had no known connections to West Africa. However, the pattern of cases showed, according to some specialists, that the virus may have been spreading outside of Africa for some months.
Instead, the authorities may suggest immunising a circle of close contacts around people who have been proven to be sick. This strategy, known as ring vaccination, has been used to contain previous outbreaks of uncommon illnesses in the past.
According to the Centers for Disease Control and Prevention (CDC), the United States has, in addition to vaccines for prevention, acquired more than two million doses of an antiviral pill known as tecovirimat. This pill is approved to treat smallpox in those who have already become infected with the disease. Additionally, the regulatory body is collaborating with the pharmaceutical company that makes the medicine in order to create an intravenous formulation.
The first case of human monkeypox was discovered in 1970 in a kid who was 9 years old and lived in an area of the Democratic Republic of the Congo that had previously been free of smallpox. The number of reported instances of monkeypox in this country has skyrocketed in the decades after widespread immunisation against smallpox was discontinued.
In 2003, the United States reported hundreds of instances of monkeypox, all of which might be linked to sick animals or household pets. Even though the virus was found for the first time in 1958 in monkeys that were being used for study, rodents are the ones responsible for spreading it.
It is believed that patients infected with the West African strain of the virus have less severe symptoms. It is not readily transmitted from person to person and has a death rate of around 4%, in contrast to a mortality rate of approximately 11% with the variant that is found in Central Africa, and a mortality rate of approximately 30% with smallpox. There have been no recorded fatalities associated with the ongoing outbreaks.
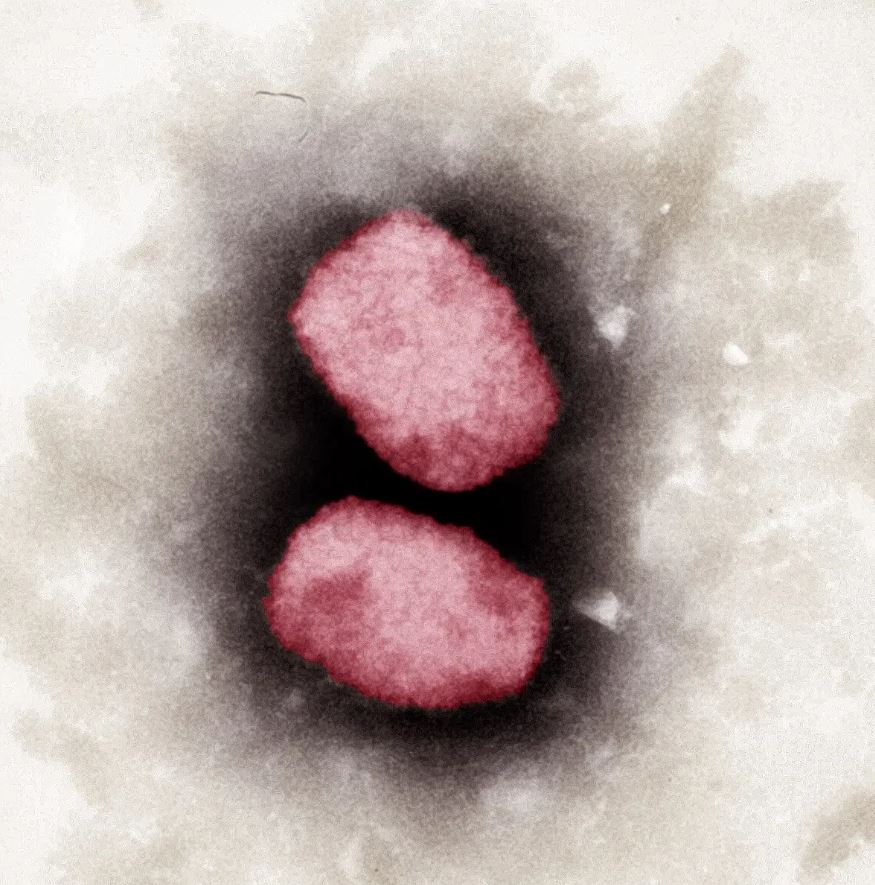
There is little evidence to suggest that the virus’s virulence or route of transmission has undergone any kind of substantial shift. The monkeypox virus is a big DNA virus that is capable of fixing its genetic faults. This is in contrast to the quickly changing coronavirus, which is based on RNA.