After being treated for a white blood cell cancer known as chronic lymphocytic leukaemia (C.L.L. ), some individuals had relapses and developed a second malignancy that no one could figure out. Were some cancer cells just resistant to treatment?
A surprising solution to this enigma has been discovered via the use of a new method known as bar coding, developed by researchers: It is not always the case that the medication targets the appropriate cells.
In their research, scientists revealed that cancer does not always develop in the mature bone marrow cells, which are where it is often found and where textbooks state that it does so. Instead, for some people, the cancer’s mother lode may be the primitive bone marrow cells, also known as stem cells, which are responsible for the production of all of the body’s white and red blood cells. Those cancer cells that are not damaged by the chemotherapy treatment have the potential to proliferate and cause a recurrence.
The finding is one of the first fruits of the bar coding approach, which is being used to help in the investigation of the causes of cancer and other illnesses. The findings are too recent to have resulted in any patient therapy. However, they are leading to startling findings that are likely to inspire revolutionary approaches to the treatment of illnesses in the near future.
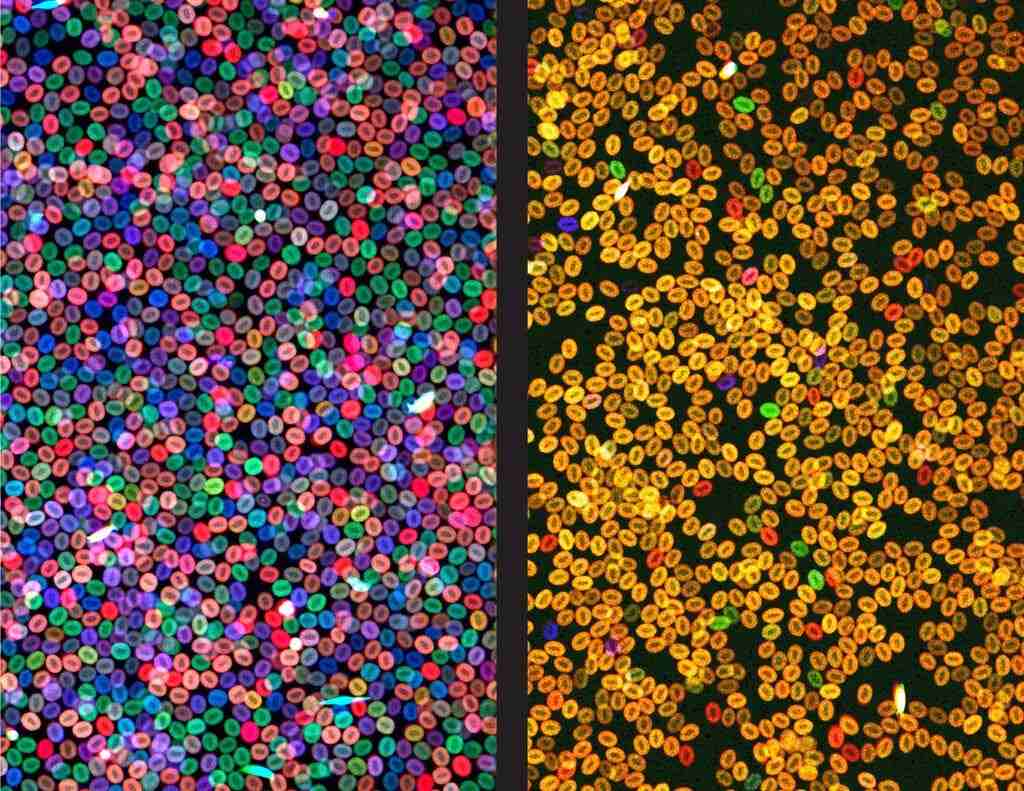
To make it work, the process involves stamping individual cells with a stamp that is then passed on to all of a cell’s descendants. Researchers may examine a cell, record its bar code, and trace the cell’s genealogy back to its parents, grandparents, great-grandparents, and ancestors — all the way back to its beginnings — since each cell that emerged from the initial bar coded cell had the same stamp as the original bar coded cell.
Dr. Jay Shendure and his colleagues at the University of Washington came up with the concept of bar coding during embryonic development, and this class of approaches was named the innovation of the year by Science magazine the following year. There are now a number of bar coding technologies available, which may be used on everything from embryonic cells to cancer cells to adult cells.
Dr. Shendure and another set of scientists at the University of Pennsylvania, for example, are utilising bar codes in mice with pancreatic cancer to track the spread of cancer cells throughout the mice’s bodies.
Dr. Vijay Sankaran of Boston Children’s Hospital and his colleagues bar coded human cancer cells by taking advantage of harmless, naturally occurring mutations that designate individual cells and are passed down through generations.
Dr. Leonard Zon of Harvard Medical School was likewise surprised by the outcome of the experiment, which was performed using the approach. The disorder clonal hematopoiesis of undetermined potential, or CHIP, was of particular interest to him. CHIP is a prevalent but poorly understood syndrome that affects elderly individuals and raises the risk of cancer and heart disease. CHIP happens when the children of a single blood stem cell take over all or a significant portion of the bone marrow, pushing out all or a significant portion of the other stem cells in the process.
The outcome was similar to what occurs in patients – by the time the fish were adults, half of their blood cells were a single hue, indicating that they were produced from a single stem cell, just as it happens in humans.
The response came as a complete surprise. The inflammatory substances released by the dominating cells were hazardous. These proteins inhibited the development of other stem cells and caused damage to the environment in which the bone marrow cells thrived. The stem cell parents, on the other hand, survived and continued to produce new toxin-secreting children.
They also discovered a gene in the mutant cells that enabled them to fight the inflammation, which was a breakthrough. When scientists removed that gene from the equation, the mutant cells were no longer able to take over.
An entirely separate issue was tackled by Fernando Camargo, a stem cell biologist at Boston Children’s Hospital, who sought to understand why typical cancer therapies that transplant healthy bone marrow stem cells from donors are so difficult, leaving patients exposed to serious infections.
Using the gene-editing tool CRISPR to genetically label marrow cells in mice, he and his colleagues found that the cells everyone thought were stem cells were not the most important contributors to the generation of red blood cells.
The majority of blood in live animals is instead produced by a distinct collection of cells, which he refers to as progenitor cells. It is possible to do a stem cell transplant using both progenitor cells and putative stem cells. Progenitor cells are transplanted, but they rapidly die off in their new environment.
Consequently, the issue is: Why do the progenitor cells fail to survive transplantation? It’s possible that the high doses of radiation and chemotherapy used to prepare the bone marrow for transplantation render the marrow unfriendly to transplantation. It’s also possible that the progenitor cells, which were infused alongside stem cells into the circulation, are unable to make their way to the bone marrow.