According to a report and testimony presented at a Senate hearing on homeland security on Wednesday, an increase in shortages of inexpensive yet essential medications is forcing hospitals to make “horrible” choices, which amounts to a threat to the nation’s security. The hearing was held on Wednesday.
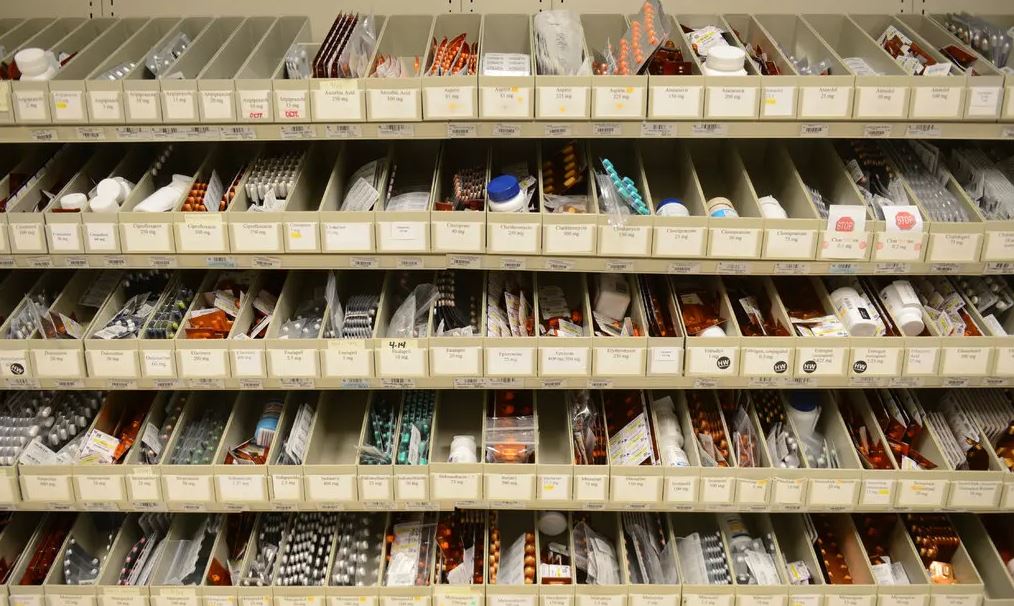
According to a study that was produced for the hearing, the number of medicine shortages grew by about 30 percent between 2021 and last year, with the average shortfall lasting 18 months and some lasting as long as 15 years. These consist of typical antibiotics, anaesthetics, and sterile fluids that are used for the purpose of maintaining the cleanliness of intravenous medication tubes.
According to Dr. Shuman, who serves in leadership positions at the hospital system of the University of Michigan and the Veterans Affairs Ann Arbor Hospital System, a well-known and relatively inexpensive cancer medication called etoposide has lately been in short supply. He had to determine which patients, young and elderly, with lung, brain, or testicular cancer, should get the restricted amount of dosages. He had to take all of these factors into consideration.
Dr. Shuman remarked, “As a physician who has spent my life to the battle against cancer, it’s impossible to convey how dreadful that is.”
The available supply was able to be stretched by the hospital pharmacy, but Dr. Shuman emphasised that pharmacists “should not be urgently attempting to squeeze out a few final drips when a life may be on the line.”
One of our specialists provided an overview of the work being done by the United States Pharmacopeia, a nonprofit organisation whose primary concern is the provision of safe drugs, to map the dynamics and causes of medication shortages. According to Vimala Raghavendran, vice president of informatics product development for the United States Pharmacopeia, that organisation discovered that there is a higher risk of shortages for medications that have a low price, a complex manufacturing process, or quality problems that have been marked by a history of recalls.
Ms. Raghavendran emphasised the need of making steps to diversify the places at which production takes place, but she also cautioned that moving production to the United States would not be the sole solution to the problem. She mentioned the recent failure of a generic medication manufacturer in the United States. The sudden shutdown of Akorn Pharmaceuticals that took place one month ago has been connected to the intensification of an existing albuterol shortage.
In addition, witnesses underlined the need of more openness regarding medicinal supply chains. According to Ms. Raghavendran, those in charge of formulating policy are “flying blind” with regard to the origins of essential components, which are often referred to as A.P.I., which stands for active pharmaceutical ingredients.
The Food and Drug Administration does receive some data on those active ingredients; however, the agency has admitted to staff members of the Senate that the data are not stored in a format that is usable; rather, the data are “buried in PDFs within individual drug applications,” according to the Senate report.
A specialist at the University of Utah who monitors medicine shortages named Erin Fox said that another information void was significant as well, and that void was that there is no data on the quality of drugmakers. This information might be put to use to recognise and encourage the most ethical suppliers, as well as to assist those suppliers in increasing their output. Despite the fact that the FDA “sees pretty obvious quality variations across products and production facilities,” this information is kept private and is not made accessible to consumers who purchase pharmaceuticals.
Dr. Fox said that there is “essentially no motivation” for any one corporation to do better than the others. There is no way for us to determine which firm performed a better job than the other even if one of them did.
She said that the issue should get attention since, in contrast to other items, people’s lives are at risk.
Eye drops that “actually save patients from going blind and cost a few dollars a month” are one example of a product that is in low supply, according to Dr. Shuman, the cancer surgeon, who also noted other alarming shortages. He indicated that surgery may be an option for glaucoma patients who did not use their eye drops on a regular basis.
According to Dr. Shuman, the fact that “drug price structures are not necessarily representative of their worth to patients” points to the need for incentives or subsidies to be provided to firms who develop these essential but inexpensive therapies that are in limited supply.