Scientists have successfully transplanted clusters of human neurons into the brains of newborn rats, a remarkable feat of biological engineering that may give more accurate models for neurological disorders such as autism and serve as a method for repairing damaged brains.
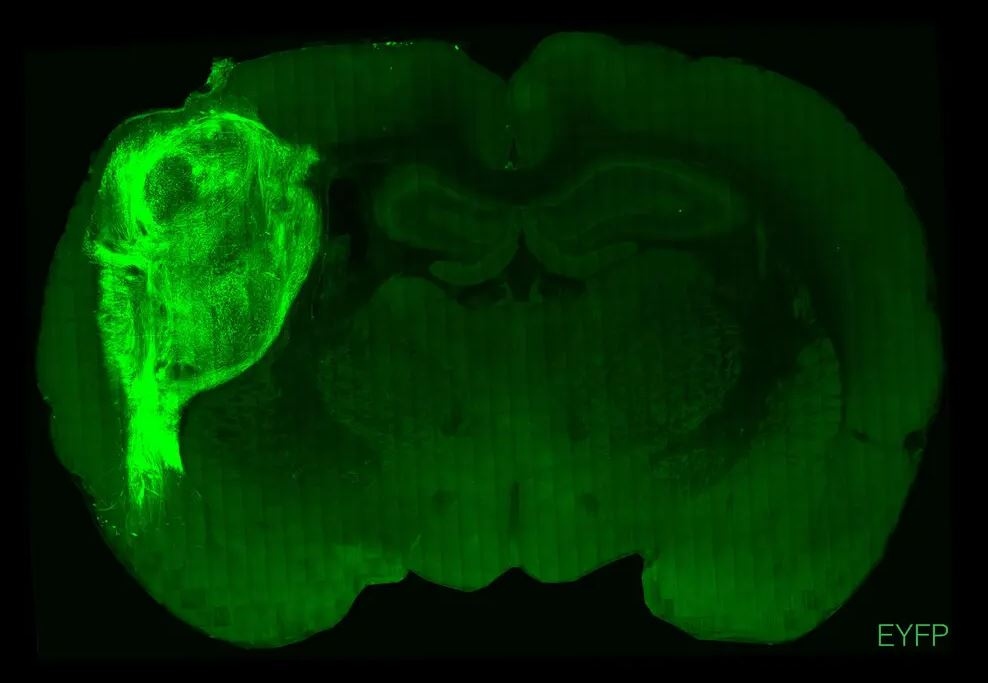
Researchers from Stanford stated in a paper released on Wednesday that clumps of human cells known as “organoids” developed into millions of new neurons and connected themselves into their new nervous systems. Once the organoids were connected to the rats’ brains, the animals were able to receive sensory impulses from their whiskers and create command signals to direct their movements.
Dr. Sergiu Pasca, the neurologist who conducted the study, said that he and his colleagues were now using the transplanted neurons to study the biology behind autism, schizophrenia, and other developmental disorders.
“If we’re going to confront the biology of these disorders, we’ll need more complicated models of the human brain,” said Dr. Pasca.
After completing medical school in Romania in 2009, Dr. Pasca joined Stanford as a postdoctoral researcher to study how to grow human neurons in a laboratory. He and his colleagues bathed the skin cells of participants with chemicals that altered their personalities. Now they resembled embryo cells, which may develop into any kind of tissue in the body.
With the addition of additional chemicals, the scientists induced the cells to transform into neurons. Then, they could witness voltage pulses travelling throughout the length of the neurons as they lay in a dish.
Dr. Pasca and his colleagues repeated the same experiment, this time using skin cells from individuals with Timothy syndrome, a rare type of autism caused by a single mutation and characterised by severe cardiac issues, language impairment, and reduced social skills.
Dr. Pasca observed a number of distinctions between Timothy syndrome neurons and conventional neurons when cultivating them in a dish. They generated increased levels of signalling molecules, such as dopamine.
However, studying single cells might only offer a limited amount of information regarding the situation. Dr. Pasca hypothesised that he might learn more by examining thousands of interconnected neurons known as brain organoids.
Dr. Pasca was able to simulate the situation of a growing brain by using a novel chemical formula. Bathed in this soup, skin cells transformed into progenitor brain cells, which then developed into the cortex, the outermost layer of the brain.
In a subsequent investigation, he and his colleagues joined three organoids: one made of brain, one built of spinal cord, and one made of muscle cells. By stimulating the organoid cortex, the muscle cells contracted.
However, organoids are not small brains. Their neurons remain underdeveloped, for one. They are also less electrically active than typical neurons in a live brain. “It is evident that these models have a lot of limitations,” Dr. Pasca added.
Scientists started placing organoids in live brains with the theory that a petri dish impeded the growth of organoids. Fred Gage and his colleagues at the Salk Institute for Biological Studies implanted human brain organoids into the adult brains of mice in 2018. The maturation of human neurons continued as the mouse brain supplied them with blood vessels.
Since then, Dr. Gage and other researchers have transplanted organoids in the back of the mouse’s brain, where visual information are processed. According to a research published online in June that has not yet been peer-reviewed, human-organoid neurons reacted to pulsating flashes of white light in a manner similar to the mouse’s own cells.
Both organoids developed in rats. However, neurons with Timothy syndrome acquired twice as many dendrites for receiving incoming impulses. In addition, dendrites were shorter.
Dr. Pasca intends to examine changes in the behaviour of rats carrying brain organoids from individuals with autism and other neurological disorders. These tests might help show how certain mutations impact brain function.
Dr. Isaac Chen, a neurosurgeon and organoid researcher at the University of Pennsylvania who was not involved in the study, recognised another potential use for the new research: the healing of human brain damage.
Dr. Chen envisioned creating brain organoids from the injured cortex of a patient’s skin. Once injected into a patient’s brain, the organoid may develop and connect to healthy neurons.